Sierra Domb, CEO & Founder of the Visual Snow Initiative, shares her journey, from having one of the world’s most unrecognised medical conditions to starting her nonprofit and researching MBCT to help manage symptoms.
A Medical Mystery
In 2015, at the age of 21, my life was irrevocably altered. Upon waking, I noticed flashing lights and moving particles in my vision, which I initially attributed to dehydration or low blood sugar. After consuming breakfast and hydrating, I anticipated that these visual disturbances would subside. However, they persisted and intensified throughout the day. While driving back to campus after a brief meal, my vision suddenly went black behind the wheel.
Although the darkness lasted only a moment, when my vision returned, it was overwhelmed by thousands of strobing lights and moving particles, resembling dense television static. Subsequently, I began experiencing additional visual and non-visual symptoms, including palinopsia, photophobia, diplopia, tinnitus, and derealisation.
In the following months, I consulted numerous doctors and specialists, but none could diagnose or explain my symptoms. After a year and a half of invasive and costly tests without answers, I began to lose hope. The severity of my condition forced me to withdraw from university, as I could no longer see clearly, work, drive, or function normally. Doctors were baffled, with some speculating about an “undiscovered condition,” while others dismissed my symptoms as psychological. The lack of a diagnosis, combined with the fear of potential blindness or worse, took a severe toll on my physical and mental health. The medical trauma and debilitating symptoms, compounded by the absence of a diagnosis, severely worsened my physical and mental health; it was agonising.
What is Visual Snow Syndrome?
I am not alone; millions worldwide endure a similar medical odyssey. The first documented cases of these symptoms appeared in 1944, but only recently was the condition named Visual Snow Syndrome (VSS). Affecting an estimated 2-3% of the global population of all ages, VSS is a neurological disorder impacting vision, hearing, sensory processing, cognition, and more. The hallmark of VSS is seeing visual snow (static, flickering dots, and flashing lights visible 24/7). Additionally, individuals with VSS often experience palinopsia, photophobia, tinnitus, depersonalisation, and migraines. A full list of VSS symptoms with photos can be found here.
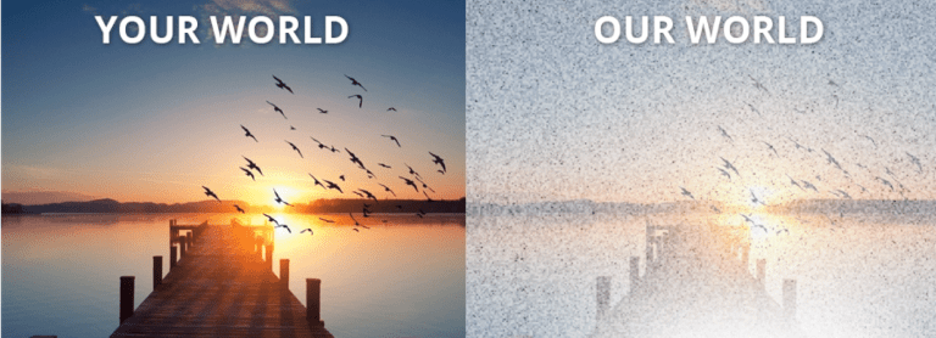
Many individuals are born with mild VSS symptoms and may unknowingly assume their perception is normal. For others, like myself, VSS can develop later in life, often without warning. Neuroimaging studies suggest that VSS is linked to abnormal hyperexcitability in the visual cortex and other sensory processing areas of the brain, as well as disruptions in neurotransmitters like glutamate and serotonin.
Devastating Global Impacts
The lack of recognition and understanding of VSS in the medical community has had devastating effects on patients. When doctors dismiss or doubt their symptoms, VSS patients often feel isolated, invalidated, and hopeless. This exacerbates their suffering, leading to severe psychological distress, including anxiety, depression, and, in extreme cases, suicidal thoughts. The resulting mental stress often worsens physical symptoms, compounding the already debilitating nature of VSS. I quickly realised that gaining medical acknowledgment of VSS was essential to preventing these tragic outcomes.
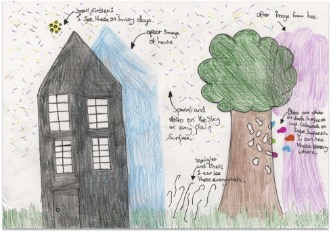
Drawing by 12 year-old girl with VSS
Taking Action & Finding Solutions
In response, I organised the first Visual Snow Conference in 2018 and founded the Visual Snow Initiative (VSI), a nonprofit organisation dedicated to raising global awareness, providing education, advocating for patients, developing treatments, and funding research for VSS. Through VSI’s efforts, we have secured a historic ICD code for VSS from the World Health Organization, achieved scientific acceptance of VSS as a distinct neurological condition, funded critical research in seven countries, and made discoveries regarding the biological basis of VSS. We have also developed the first Diagnostic Criteria for VSS, created a Global Directory of VSS Physicians, produced educational videos, and established resources to improve communication, health literacy, and education regarding VSS.
Research on MBCT for VSS
To date, VSI has heard from individuals affected by VSS in over 93 countries, most of whom are seeking treatment for themselves or a loved one. Until recently, no effective treatments existed, with previous medications often causing side effects or worsening symptoms. As we continue to research VSS and work towards a cure, we explore various promising modalities to improve symptoms and quality of life. One such intervention is Mindfulness-Based Cognitive Therapy (MBCT). Neurologist and neuro-ophthalmologist Dr. Sui Wong, author of Mindfulness for Brain Health, approached VSI to study the effectiveness of MBCT for VSS, marking the first time MBCT has been researched in this patient population. Dr. Wong’s study, conducted in collaboration with VSI and Guy’s and St Thomas’ NHS Foundation, used a protocol developed by the gold standard for mindfulness teachings: Oxford Mindfulness.
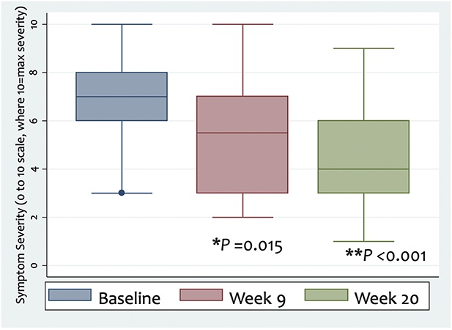
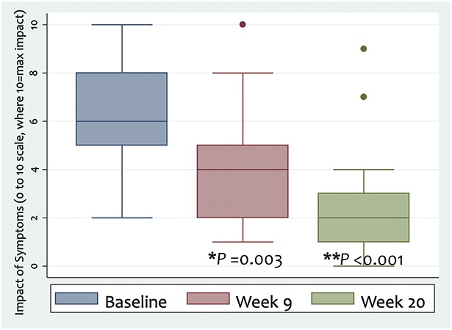
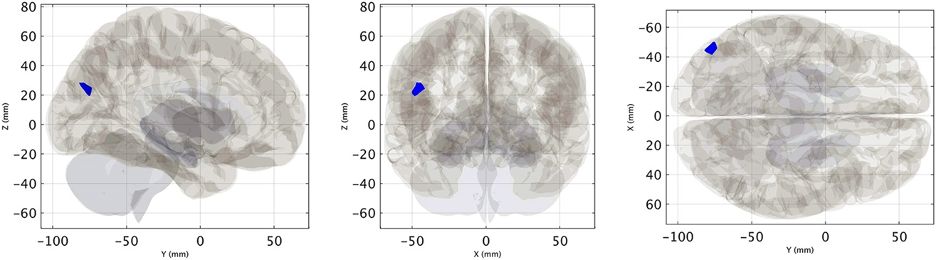
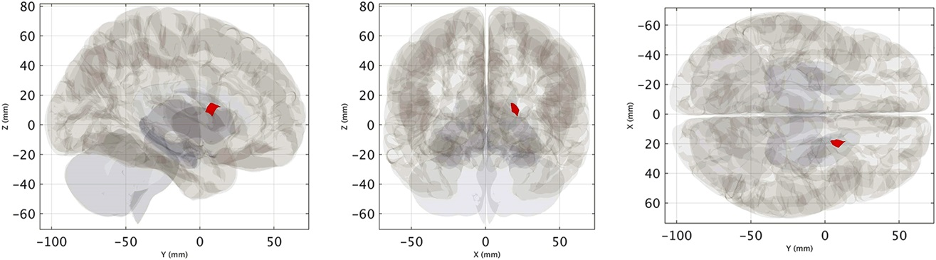
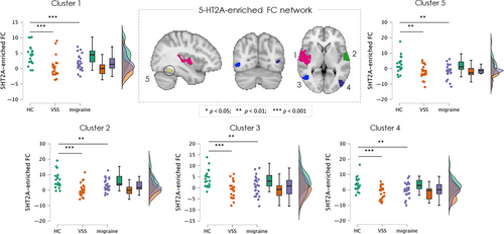
Dr. Wong’s feasibility study, published in the Journal of Neuro-Ophthalmology, demonstrated that MBCT can reduce both visual and non-visual symptoms of VSS and improve quality of life. Functional MRI (fMRI) scans revealed significant measurable changes in brain activity, indicating that MBCT can modulate the dysfunctional visual networks associated with VSS. This objective evidence was reinforced by study participant reports. The study’s findings suggest that MBCT not only alleviates symptoms but also brings about material changes in the underlying neurological condition.
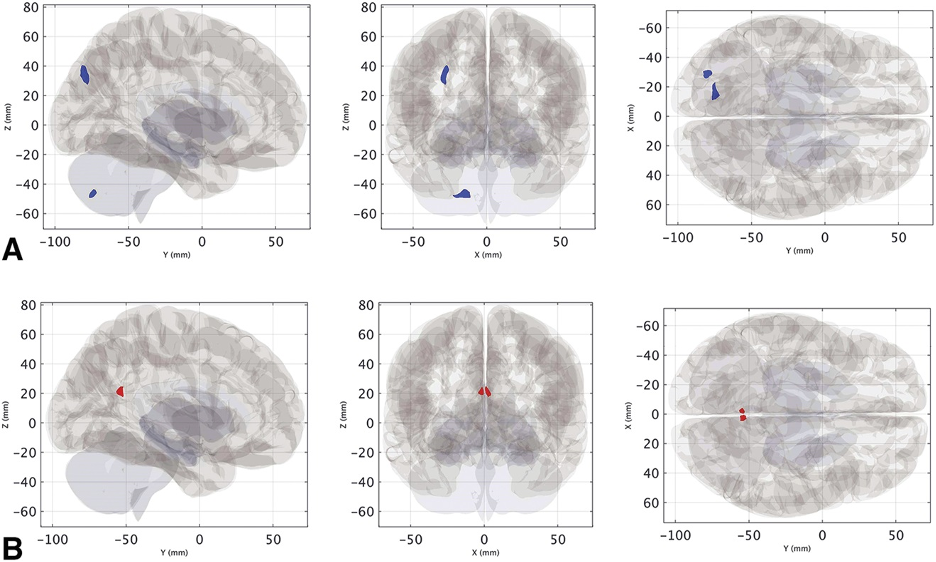
VSS is linked to dysregulation in the brain’s visual networks, causing a constant “noise-like” perception. This dysfunction also impacts attentional and salience networks; fMRI brain scans before and after MBCT reveal significant changes in these networks. By targeting the brain’s visual and extravisual networks, MBCT can reduce visual disturbances like visual snow/static and enhance cognitive functions related to attention and emotional regulation. Additionally, its ability to alleviate stress and anxiety, related to VSS, can improve patients’ quality of life.
Though VSS is not a psychiatric disorder, the success of MBCT highlights the importance of targeting neuroplasticity and functional connectivity in treating neurological conditions like VSS. Mindfulness can help promote new neural connections, calm the stress response, enhance sensory processing, and regulate neurotransmitters like serotonin, which, along with glutamate, are crucial in managing VSS.
Dr. Wong presented her findings at the NANOS Conference, gaining strong support from the neuroscience community and VSS expert Dr. Owen White. While VSS currently has no cure, MBCT shows promise as a noninvasive intervention that targets and modulates dysfunctional brain pathways to reduce symptoms. Originally developed for psychological conditions, MBCT’s scope has expanded to effectively manage neurological disorders like VSS, acting as a brain retraining mechanism to induce functional changes and lessen symptom severity.
To learn more about Dr. Wong’s MBCT for VSS research, please visit the MBCT-vision website.
The Role of Mindfulness & MBCT in Neurological Conditions
Mindfulness and MBCT are increasingly recognised for their ability to calm a hyperexcitable nervous system, which is crucial in managing conditions like VSS. VSS is linked to hyperactivity in the visual cortex and abnormalities in neural signals between the eyes and brain. This hyperactivity can lead to a range of symptoms, including chronic pain and sensory disturbances.
Mindfulness and MBCT work by modulating the autonomic nervous system (ANS), shifting it from an overactive “fight or flight” mode to a more balanced state. This shift reduces nervous system excitability, leading to improvements in symptoms such as visual disturbances, sensory overload, and emotional distress. Neuroimaging studies show that mindfulness decreases activity in the amygdala, which regulates stress, and enhances connectivity in the prefrontal cortex, which manages executive functions and emotional regulation.
By restoring balance in the ANS and improving brain connectivity, mindfulness and MBCT offer an effective approach to managing neurological and neuro-ophthalmological conditions, ultimately enhancing patients’ quality of life.
My Experience with MBCT
Before beginning MBCT, I had already seen significant improvement in my visual symptoms and quality of life through Neuro-Ophthalmologic Rehabilitation Therapy. However, I continued to struggle with persistent non-visual symptoms such as anxiety, depression, depersonalisation, insomnia, and brain fog. Motivated by the scientific evidence from Dr. Wong’s study, I decided to try her protocol, which mirrored the Oxford Mindfulness curriculum, in hopes of further relief.
My experience with MBCT was unexpectedly transformative. Over two months, I diligently practiced the mindfulness programme, albeit with some necessary adjustments to suit my schedule. These sessions significantly alleviated my non-visual symptoms, and I was pleasantly surprised to find that my visual symptoms, including visual snow, also improved. MBCT also provided me with practical tools to manage catastrophic thinking, which had been a significant challenge, especially given the PTSD I developed due my traumatic VSS medical odyssey. MBCT not only addressed my symptoms but also made me feel better physically and mentally. The skills and insights gained continue to help me navigate both VSS and broader life challenges.
Ultimately, scientific evidence, including fMRI imaging showing measurable brain changes, patient reports of symptom reduction, and my personal experience, have reinforced MBCT as a powerful tool for managing overall health, particularly in neurological conditions like VSS.
“MBCT not only addressed my symptoms but also made me feel better physically and mentally.”
Demystifying Primitive Notions about Mindfulness
In addition to leading VSI and serving on the International Advisory Board for the Columbia-WHO Collaborating Centre for Global Mental Health, I have an academic background in behavioural science, health, and multicultural communication. I also got my CITI-certification in Human Subjects Research with a focus on Social-Behavioural-Educational Research, specialising in qualitative data analysis.
While I approach research and medicine from a scientific, evidence-based perspective, I initially held some reservations about mindfulness prior Dr. Wong’s study, uninformed if it was medically accepted or physiological changes could occur. However, there was in fact compelling scientific evidence and the severity of my symptoms led me to maintain an open mind. Addressing these misconceptions is important, as others may share them and mistakenly view mindfulness as lacking scientific credibility.
The term “mindfulness” often carries a stigma due to its ties to spiritual or holistic wellness, leading to scepticism among those who favour empirical science and pharmacological treatments. However, mindfulness is increasingly recognised by the medical community as a scientifically valid approach with substantial therapeutic potential, particularly for neurological conditions. Research, including fMRI studies, has shown that mindfulness can induce measurable changes in brain function, particularly in regions involved in sensory processing, emotional regulation, and attention.
Mindfulness promotes neuroplasticity, forming new neural connections and regulating neurotransmitters like serotonin and cortisol, essential for treating neurological conditions. Supported by objective evidence, clinical trials, brain imaging, and meta-analyses, mindfulness and MBCT have shown benefits for conditions like VSS, chronic pain, migraines, and neurodegenerative diseases.
The growing acceptance of mindfulness in modern medicine reflects its transition from traditional practices to a scientifically supported intervention integrated into evidence-based protocols. Just as VSS was once dismissed as not a real condition but is now recognised with its own ICD code by the World Health Organization, I encourage people to keep an open mind and recognise that medicine can evolve with new scientifically valid evidence.
“…mindfulness is increasingly recognised by the medical community as a scientifically valid approach with substantial therapeutic potential, particularly for neurological conditions.”
The Future

Investing in the health of our mind and nervous system benefits not just those with medical conditions like VSS, but also anyone seeking overall well-being, as physical and mental health are deeply connected. The protocol used in Dr. Wong’s VSS and MBCT study, established by Oxford Mindfulness, highlights the importance of global accessibility, collaboration, education, and support for mindfulness initiatives. Research continues to show the value of mindfulness, which can be broadly implemented, even in resource-limited countries. Dr. Wong’s work, along with ongoing studies like VSI’s Randomised Control Trial, represents a significant advance in effectively managing VSS.
The Visual Snow Initiative and Oxford Mindfulness are working together to expand global access to mindfulness interventions and related courses.
For more information, research, and resources regarding VSS, please visit the Visual Snow Initiative website.
References
Brewer, J.A., et al., 2011. Meditation Experience Is Associated With Differences in Default Mode Network Activity and Connectivity. Proceedings of the National Academy of Sciences, 108(50), pp.20254-20259.
Carroll, F.D., 1944. Visual Symptoms Caused by Digitalis. Transactions of the American Ophthalmological Society, 42, pp.243-249.
Cherkin, D.C., et al., 2016. Effect of Mindfulness-Based Stress Reduction vs Cognitive Behavioral Therapy or Usual Care on Back Pain and Functional Limitations in Adults with Chronic Low Back Pain: A Randomized Clinical Trial. JAMA, 315(12), pp.1240-1249.
Farb, N.A.S., et al., 2010. Minding One’s Emotions: Mindfulness Training Alters the Neural Expression of Sadness. Emotion, 10(1), pp.25-33.
Gotink, R.A., et al., 2016. Standardised Mindfulness-Based Interventions in Healthcare: An Overview of Systematic Reviews and Meta-Analyses of RCTs. PLoS ONE, 10(4), e0124344.
Grossman, P., et al., 2010. MS Quality of Life, Depression, and Fatigue Improve After Mindfulness Training: A Randomized Trial. Neurology, 75(13), pp.1141-1149.
Hofmann, S.G., Sawyer, A.T., Witt, A.A., and Oh, D., 2010. The Effect of Mindfulness-Based Therapy on Anxiety and Depression: A Meta-Analytic Review. Journal of Consulting and Clinical Psychology, 78(2), pp.169-183.
Hölzel, B.K., et al., 2011. How Does Mindfulness Meditation Work? Proposing Mechanisms of Action From a Conceptual and Neural Perspective. Perspectives on Psychological Science, 6(6), pp.537-559.
Lauschke, J.L., Plant, G.T., and Fraser, C.L., 2016. Visual Snow: A Thalamocortical Dysrhythmia of the Visual Pathway? Journal of Clinical Neuroscience, 28, pp.123-127.
Lawrence, M., Booth, J., Mercer, S., and Crawford, E., 2013. A Systematic Review of the Benefits of Mindfulness-Based Interventions Following Transient Ischemic Attack and Stroke. International Journal of Stroke, 8(6), pp.465-474.
Lomas, T., Ivtzan, I., and Fu, C.H.Y., 2015. A Systematic Review of the Neurophysiology of Mindfulness on EEG Oscillations. Neuroscience & Biobehavioral Reviews, 57, pp.401-410.
Pickut, B.A., et al., 2013. Mindfulness-Based Intervention in Parkinson’s Disease Leads to Structural Brain Changes on MRI: A Randomized Controlled Longitudinal Trial. Clinical Neurology and Neurosurgery, 115(12), pp.2419-2425.
Puledda, F., Dipasquale, O., Gooddy, B.J.M., Karsan, N., Bose, R., Mehta, M.A., Williams, S.C.R. and Goadsby, P.J., 2023. Abnormal Glutamatergic and Serotonergic Connectivity in Visual Snow Syndrome and Migraine with Aura. Annals of Neurology, 94(5), pp.873-884.
Scholz, J., et al., 2009. Training Induces Changes in White-Matter Architecture. Nature Neuroscience, 12(11), pp.1370-1371.
Schankin, C.J., et al., 2014. ‘Visual Snow’: A Disorder Distinct from Persistent Migraine Aura. Brain, 137(5), pp.1419-1428.
Segal, Z.V., Williams, J.M.G., and Teasdale, J.D., 2002. Mindfulness-Based Cognitive Therapy for Depression: A New Approach to Preventing Relapse. Guilford Press.
Segal, Z.V., et al., 2010. Antidepressant Monotherapy vs Sequential Pharmacotherapy and Mindfulness-Based Cognitive Therapy, or Placebo, for Relapse Prophylaxis in Recurrent Depression. Archives of General Psychiatry, 67(12), pp.1256-1264.
Simpson, J. C., Goadsby, P. J., & Prabhakar, P. (2013). Positive persistent visual symptoms (visual snow) presenting as a migraine variant in a 12-year-old girl. Pediatric neurology, 49(5), 361–363.
Simpson, R., Mair, F.S., and Mercer, S.W., 2018. Mindfulness-Based Stress Reduction for People with Multiple Sclerosis–A Feasibility Randomized Controlled Trial. BMC Neurology, 18(1), pp.1-9.
Tang, Y.Y., et al., 2009. Central and Autonomic Nervous System Interaction Is Altered by Short-Term Meditation. Proceedings of the National Academy of Sciences, 106(22), pp.8865-8870.
Tang, Y.Y., Hölzel, B.K., and Posner, M.I., 2015. The Neuroscience of Mindfulness Meditation. Nature Reviews Neuroscience, 16(4), pp.213-225.
Tsang, T., Shidlofsky, C. and Mora, V., 2022. The efficacy of neuro-optometric visual rehabilitation therapy in patients with visual snow syndrome. Frontiers in Neurology, 13.
Wells, R.E., et al., 2014. Meditation for Migraines: A Pilot Randomized Controlled Trial. Headache: The Journal of Head and Face Pain, 54(9), pp.1484-1495.
Wong, S.H., et al., 2023. Visual Snow Syndrome Improves With Modulation of Resting-State Functional MRI Connectivity After Mindfulness-Based Cognitive Therapy: An Open-Label Feasibility Study. Journal of Neuro-Ophthalmology.
Wong, S.H., Pontillo, G., Kanber, B., Prados, F., Wingrove, J., Yiannakas, M., Davagnanam, I., Gandini Wheeler-Kingshott, C.A.M., and Toosy, A.T., 2024. Visual Snow Syndrome Improves With Modulation of Resting-State Functional MRI Connectivity After Mindfulness-Based Cognitive Therapy: An Open-Label Feasibility Study. Journal of Neuro-Ophthalmology, 44(1), pp.112-118. DOI: 10.1097/WNO.0000000000002013.
Zeidan, F., et al., 2012. Mindfulness Meditation-Related Pain Relief: Evidence for Unique Brain Mechanisms in the Regulation of Pain. Neuroscience Letters, 520(2), pp.165-173.




